Triggers, Risk Factors, and Causes of Atrial Fibrillation
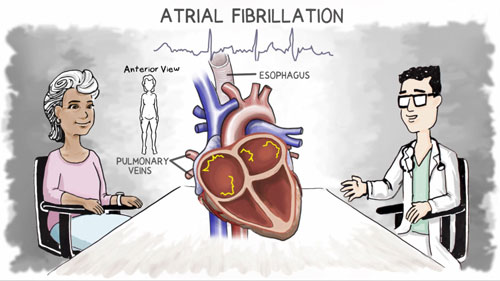
Where in the Heart Does Atrial Fibrillation Begin?
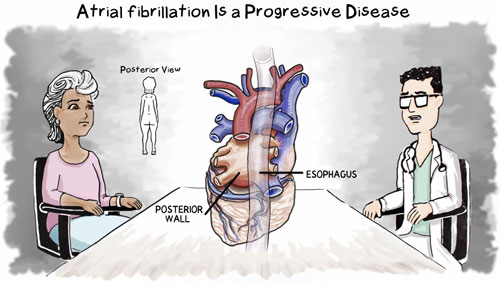
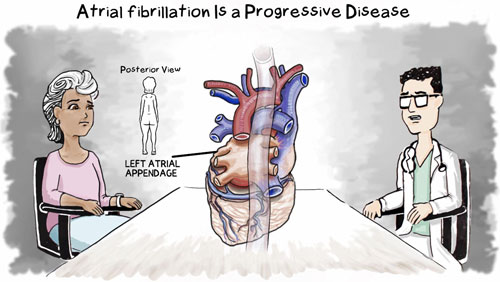
There are three areas of the heart where atrial fibrillation normally starts.
- Pulmonary Veins: Most of the time atrial fibrillation begins near the pulmonary veins. These are the veins that move oxygen-rich blood from the lungs to the heart. There are 4 main pulmonary veins. Each of the lungs has 2 pulmonary veins that connect to the left atrium.
- Posterior Wall of the Atrium: Atrial fibrillation also begins on the back, or posterior, wall of the atrium.
- Left Atrial Appendage: The left atrial appendage (LAA) is another area of the heart where atrial fibrillation begins.1 The LAA is a small pouch found at the top of the left atrium. The LAA may be linked to persistent atrial fibrillation in particular.1
What Conditions Lead to Higher Risk of Atrial Fibrillation?
A number of medical conditions can put someone at higher risk for atrial fibrillation.
Diabetes, which has greatly increased in the population, is linked to higher rates of atrial fibrillation. The glucose (blood sugar) imbalance that occurs with diabetes can directly affect the tissues of the heart.2
Each time you’re suddenly awakened by lack of oxygen from sleep apnea, it stresses the heart. It can also cause chemical changes inside the heart. Treating the sleep apnea can often improve a person’s atrial fibrillation.
An overactive thyroid gland is called hyperthyroidism. The thyroid gland, in your neck, makes hormones. If the thyroid is too active, it increases the heart rate. Atrial fibrillation is the most common heart problem in people with an overactive thyroid.
Atrial fibrillation is the most common abnormal heart rhythm associated with infections. This is because infections can cause inflammation in the body. This, in turn, can cause changes in the heart. The extent of the infection determines its effect on the heart.3 For example, widespread infection, called sepsis, takes a toll on the heart and all organs of the body.
Being obese puts a person at higher risk for atrial fibrillation. If you are in this category, check with your health care provider about the healthiest ways to lose weight.
Many cardiovascular conditions predispose people to develop atrial fibrillation. (Cardiovascular refers to the heart or blood vessels or both.) The following are some of the most common cardiovascular problems that can lead to atrial fibrillation.
Someone with long-term high blood pressure is at risk for atrial fibrillation. Here are the numbers showing the various levels of high blood pressure. High blood pressure has other negative health effects, too. Be sure to have your blood pressure checked regularly. And talk to your health care provider right away if you have high blood pressure.
| Category of Blood Pressure | Upper Number (Systolic Pressure) |
Lower Number (Diastolic Pressure) |
|
| Normal | < 120 | and | < 80 |
| Elevated | 120-129 | and | < 80 |
| High Stage 1 | 130-139 | or | 80-89 |
| High Stage 2 | ≥ 140 | or | ≥ 90 |
| Critically High | > 180 | and/or | > 120 |
Two main types of heart valve disease can put people at higher risk for atrial fibrillation.
Mitral valve stenosis: Stenosis is a stiffening of the heart valve. The mitral valve opens to allow blood to flow from the left atrium (heart's upper chamber on the left side) into the left ventricle (lower chamber on the left side). As the valve thickens, the opening narrows. As a result, too little blood is going from the atrium into the ventricle.
Mitral regurgitation: If the flaps of the mitral valve don't fully close, some blood can seep back into the atrium. This is called regurgitation.
In addition, a diseased valve sometimes needs to be replaced. Someone who has had a valve replacement is also at higher risk for atrial fibrillation.
Coronary artery disease (CAD) occurs when the arteries that send blood to your heart muscle become blocked. This happens as plaque builds up inside the arteries. Plaque is made up of fatty substances, such as cholesterol, in your blood. Because of the plaque, less blood can flow through your arteries, and the heart muscle cannot get enough blood and oxygen. This can affect heart function.
Experts agree that CAD is a risk factor for atrial fibrillation.4
A heart attack results from untreated coronary artery disease, or CAD. When the heart’s arteries become almost fully blocked, very little blood flows to the heart muscle. As a result, a heart attack occurs. During a heart attack, a small portion of the heart tissue dies from lack of oxygen. In some cases the heart attack damages tissues in the atrium. Just as CAD is a risk factor for developing atrial fibrillation, a heart attack is, too.
Congenital means “present from birth.” So congenital heart disease (CHD) is a heart abnormality that has existed since birth. About 1% of babies are born with some type of CHD. CHD may take the form of:5
- Abnormal position of the blood vessels in the heart
- A defect or hole in the heart septum, which is the tissue that separates the heart’s chambers
- Heart valve abnormalities
In most cases, people with CHD won’t develop atrial fibrillation until adulthood. However atrial fibrillation is a well-established, chronic problem in adults older than age 50 who have CHD.6
Heart failure is another heart condition that can lead to atrial fibrillation.
What Else Can Potentially Cause Atrial Fibrillation?
There are a number of other factors that can increase a person’s risk of developing atrial fibrillation. The following are not medical conditions, but they are linked to higher rates of atrial fibrillation.
| Aging | The risk of atrial fibrillation increases as people age, especially after age 65. (Atrial fibrillation is rare in children. However it does occur, especially children who have had heart surgery or who are obese.) |
| Family History and Genetics | If a family member has had atrial fibrillation, you have a higher risk of it, too. In fact, researchers have found genetic mutations that increase a person’s risk of atrial fibrillation. |
| Stress | Emotional stress, including panic disorders, can also put someone at higher risk of atrial fibrillation. Talk to your health care provider about ways you can reduce stress. |
| Alcohol | Alcohol consumption—and especially binge drinking—raises a person’s risk of atrial fibrillation. For some people, even modest amounts of alcohol can trigger atrial fibrillation. |
| Caffeine | Caffeine increases your heart rate, which can trigger atrial fibrillation. Caffeine is found in coffee, of course. It is also in black tea, certain energy drinks and soft drinks, and chocolate. |
| Smoking | Scientists have found that smoking increases the risk of atrial fibrillation. One reason for this is that smoking increases your heart rate. In addition, the risk seems to increase for long-term smokers. But the risk lowers if you quit. Exposure to secondhand smoke, even in the womb, can also increase a child’s risk for atrial fibrillation. |
| Skipping Medications | You should always take prescription medication as directed. This is critical for anyone taking medication for atrial fibrillation. |
| Taking Stimulants or Street Drugs | Stimulants, for example many diet pills, cause the heart to race. The same is true for street drugs like cocaine or methamphetamines (meth). These drugs can either trigger atrial fibrillation or worsen it. They can also cause other dangerous heart rhythms in the ventricles. |
A person has no control over the first few items on the list: age and family history. In addition, people often learn ways to reduce stress in their lives.
Many of the remaining factors that can trigger atrial fibrillation, however, are within your control. Talk to your health care provider about how to lead a healthy lifestyle.
If you are diagnosed with atrial fibrillation, find out why treatment is so important.
- Di Biase, L., Natale, A., Romero, J. (2018). Thrombogenic and arrhythmogenic roles of the left atrial appendage in atrial fibrillation. Circulation, 138, 2036-2050. https://doi.org/10.1161/CIRCULATIONAHA.118.034187
- Sun, Y., & Hu, D. (2010). The link between diabetes and atrial fibrillation: cause or correlation?. Journal of cardiovascular disease research, 1(1), 10–11. https://doi.org/10.4103/0975-3583.59978
- Gundlund, A., Bjerring Olesen, J., Butt, J.H., Aagaard Christensen, M., Gislason, G.H., Torp-Pedersen, C., Køber, L., Kümler, T., Loldrup Fosbøl, E. (2020). One-year outcomes in atrial fibrillation presenting during infections: a nationwide registry-based study. European heart journal, 41(10), 1112–1119. https://doi.org/10.1093/eurheartj/ehz873
- Brandes, A., Smit, M.D., Nguyen, B.O., Rienstra, M., Van Gelder, I.C. (2018). Risk factor management in atrial fibrillation. Arrhythmia & electrophysiology review, 7(2), 118-127. https://doi.org/10.15420/aer.2018.18.2
- Mandalenakis, Z., Rosengren, A, Lappas G., Eriksson, P., Gilljam, T., Hansson, P., Skoglund, K., Fedchenko, M., Dellborg, M.(2018). Atrial fibrillation burden in young patients with congenital heart disease. Circulation, 137, 928-937. https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.117.029590
- Labombarda, F., Hamilton, R., Shohoudi, A., Aboulhosn, J., Broberg, C.S., Chaix, M.A., Cohen, S., Cook, S., Dore, A., Fernandes, S.M., Fournier, A., Kay, J., Macle, L., Mondésert, B., Mongeon, F.P., Opotowsky, A.R., Proietti, A., Rivard, L., Ting, J., Thibault, B., Zaidi, A., Khairy, P. (2017). Increasing prevalence of atrial fibrillation and permanent atrial arrhythmias in congenital heart disease. Journal of the American College of Cardiology, 70(7), 857-865. doi: 10.1016/j.jacc.2017.06.034

